If you have low testosterone (T), then testosterone replacement therapy (TRT) might be the best option to alleviate your symptoms and improve the quality of your life.
However, the treatment is not free of adverse reactions. If your doctor has suggested TRT for your condition, then he or she will also warn you about the possible side effects of the therapy.
One of these effects is an increase in your red blood cell count. This can be seen as a benefit for those with low T and anemia.
However, some patients experience an increase above the normal references in several blood parameters which can lead to complications.
How does testosterone affect hemoglobin and hematocrit levels?
Currently, there is a lack of consensus on whether testosterone therapy increases the risk of blood clots. A large meta-analysis of more than 30 randomized studies has found no association between testosterone therapy and heart attacks or stroke.
Hemoglobin and hematocrit levels can be elevated due to decreased blood volume, such as during dehydration. According to studies, testosterone therapy leads to a 7–10% increase in hemoglobin and hematocrit.
If it increases above 54%, it can be a risk factor for the development of blood clots, which can lead to heart attack or stroke.
Hemoglobin – an iron-containing protein in your erythrocytes that allows blood to transport the oxygen in your body.
Hematocrit – a volume of all erythrocytes compared to your total blood volume. It reflects on the ratio between the cells and the liquid portion of your blood.
Furthermore, clots that form in the veins (venous thrombosis) can break loose and plug into a vessel in the lungs or the brain. This leads to another potentially fatal condition called venous thromboembolism.
Are testosterone boosters safer?
Testosterone boosters such as Andro 400 or supplements do not appear to be a safer or more effective option for patients with low T. They usually contain various herbal extracts with poor scientific support for their effectiveness.
A recent analysis that evaluated 50 testosterone boosters and their ingredients found that more than 75% had no evidence to support their claims. Furthermore, research suggests that in 10% of the cases, some of the ingredients might actually lower T.
Despite being natural, the safety of herbal testosterone enhancers also remains unclear. There have been cases of thromboembolism likely caused by the use of certain extracts.
How does testosterone treatment increase hemoglobin?
Testosterone therapy increases hemoglobin, and men with baseline hematocrit levels above 48-50% are at an increased risk of polycythemia.
One of the mechanisms by which testosterone can lead to polycythemia is via increasing iron utilization. It affects a protein in your body called hepcidin which normally reduces iron absorption.
By suppressing it, testosterone increases the availability of iron which raises hemoglobin production.
Hepcidin suppression is most significant during the first month of therapy. On the other hand, it takes about 3-6 months to cause high hemoglobin and high hematocrit levels.
Elevated hemoglobin might be associated with certain risks including atherosclerosis and related cardiovascular incidents.
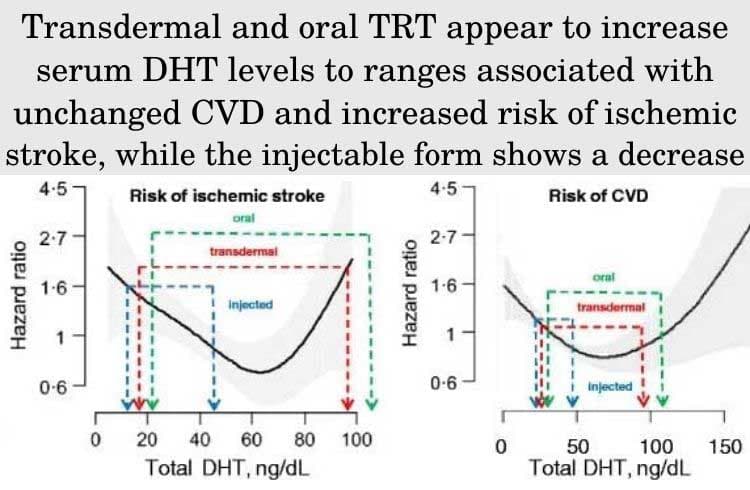
However, not all forms of testosterone appear to affect the risk of heart attack or stroke. According to a meta-analysis that included data from 3703 patients, oral forms of TRT can increase the risk of cardiovascular events. On the other hand, injections were not associated with an increased risk.
Other concerns due to high hemoglobin levels such as erectile dysfunction are not supported by scientific evidence. In fact, patients with ED are more likely to have anemia (low hemoglobin).
How to lower hematocrit while on testosterone therapy
Prevent dehydration
Avoiding dehydration is important, as it can lead to an elevation in the value of your hematocrit that is unrelated to your TRT.
If you are well hydrated and your hematocrit levels are above 54%, then official guidelines recommend discontinuing the testosterone treatment until your values return to baseline.
Donate blood
The condition can also be treated via therapeutic venesection, which means drawing blood out of your body. Being on TRT does not prevent you from donating blood so unless you are taking other medications as well, donation might be an option.
However, regular blood donation might not be the best strategy to manage the condition, because it further stimulates erythropoiesis. Scientific evidence suggests that regular blood donation is an insufficient method to maintain a hematocrit below 54%.
Quit smoking
Smokers are at an increased risk for increased hematocrit. The risk can be reduced by smoking cessation.
Read next – “How Smoking Affects Testosterone Levels“
If there is an increased risk of thrombi, aspirin can be taken for its antithrombotic effects. However, the risk for bleeding and gastrointestinal side effects must be carefully evaluated by a medical doctor.
Get a free consultation with our medical expert for any questions about hormone replacement therapy