Testosterone stimulates the process of red blood cell (erythrocyte) production called erythropoiesis. The effect is dose-dependent but the exact mechanisms are not fully known yet.
If your erythrocyte count increases above normal levels, the condition is called erythrocytosis. It is usually accompanied by elevated total hemoglobin (above 18.5 g/dL) and high hematocrit (over 54%). The combination of these signs is defined as polycythemia.
How does testosterone affect red blood cell production?
Testosterone is proven to stimulate the production of erythropoietin (EPO). That is a hormone produced by your kidneys that stimulates normal red blood cell production.
Elevated red blood cell count is usually accompanied by a rise in hemoglobin and leads to increased hematocrit.
Erythropoietin is increased most significantly during the first month of testosterone therapy. However, it returns to baseline after the 6th month of continuous TRT.
On the other hand, it takes 3-6 months for the red blood cell count to rise due to testosterone. This process is slower in patients with low T who also suffer from anemia.
Besides, blood parameters peak later and are higher in older individuals. While younger men on TRT had a significantly lower risk for erythrocytosis and high hematocrit.
How to lower red blood cell count while on TRT
Polycythemia is reversible, and if you get erythrocytosis or a high hematocrit, discontinuing TRT will resolve the problem. Since the effect is dose-dependent, testosterone therapy can be reinitiated, with a lower starting dose.
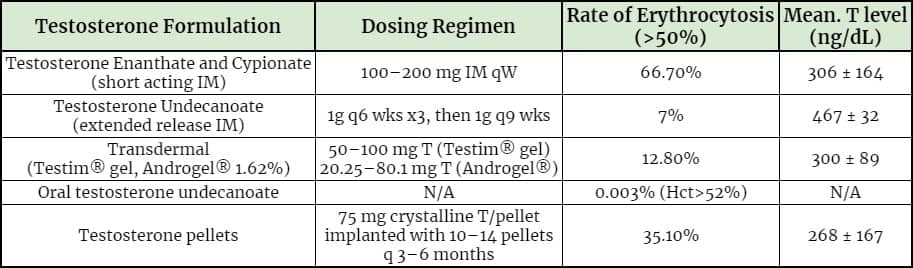
Evidence suggests that short-acting forms of testosterone might be more likely to cause erythrocytosis compared to other forms.
66.7% of patients experience an increase in hematocrit levels above 50% when treated with short-acting testosterone injections such as testosterone cypionate and enanthate.
Only 7% of patients on therapy with long-acting testosterone undecanoate injections have hematocrit above 50%. Patients on testosterone gel or pellets experience elevated hematocrit in 12.8% and 35.1% of the cases respectively.
That might be because a sudden rise in T levels can lead to a stronger erythropoietin response from kidneys. A lower initial dose and a more stable administration routine might prevent the reoccurrence of erythrocytosis.
Does testosterone therapy confer risk for venous thromboembolism?
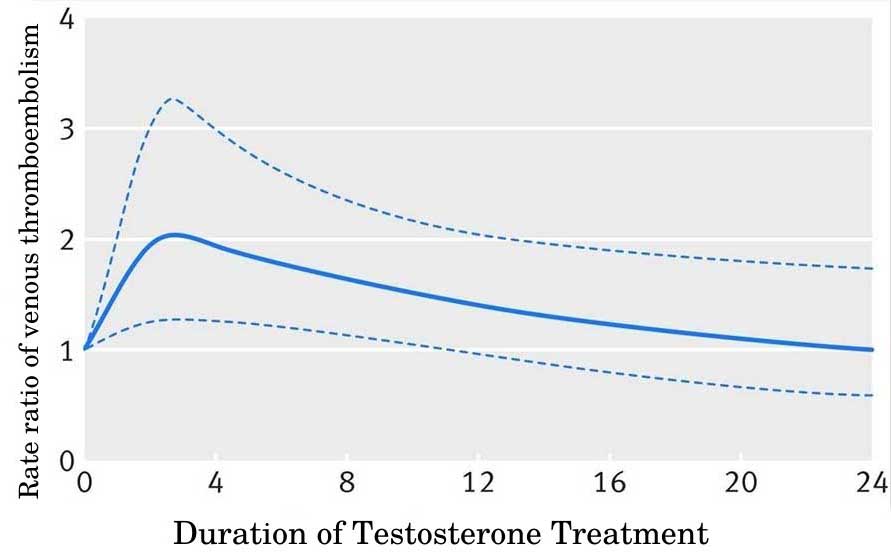
Currently, there is insufficient evidence on whether TRT increases the risk for venous thromboembolism. Nevertheless, patients prone to polycythemia might be at an increased risk only during the first 6 months of therapy.
Testosterone treatment may increase the risk of thromboembolism from 0.16% to 0.26% only for the first six months. After the first six months, the risk returns to baseline.
That’s likely because the effects of testosterone on erythropoiesis and hemoglobin production are transitory.
There are also studies that have reported no associations between TRT and increased risk of venous thromboembolism.
Patients who are at an increased risk of polycythemia or thrombi include chronically ill patients, suffering from:
- COPD (chronic obstructive pulmonary disease)
- Obstructive sleep apnea
- Thrombophilia
- Immobility or prolonged bed rest
- Obesity
- Congestive heart failure
- Prior venous thromboembolism or family history of such events
Patients who take blood thinners might actually be at a higher risk of bleeding and hemorrhages when combining them with TRT.
In addition, testosterone enhances the anticoagulant effect. Make sure to consult with your doctor as the dosage of your medication might require a correction.
Get a free consultation with our medical expert for any questions about hormone replacement therapy