Testosterone replacement therapy (TRT) has been a widely accepted treatment for male hypogonadism for decades. However, the treatment is still FDA-approved for use in women due to a lack of research on its safety and effectiveness.
Nevertheless, testosterone (T) can be legally prescribed as an off-label therapy for women, and its use amongst females has grown in popularity in recent years. A major contributing factor to that trend is the increased use of TRT amongst female-to-male (FTM) patients.
The growing popularity has also led to the publication of numerous studies on FTM patients, which reveal that testosterone therapy can be well-tolerated by the female body, even in supraphysiological doses.
Furthermore, there is some evidence to suggest that using physiological doses of testosterone amongst women with medical conditions may provide benefits that far outweigh the risks. Examples may include peri and postmenopausal symptoms, hypoactive sexual desire disorder and many others.
Therefore, TRT may offer a safe and effective treatment for females with various symptoms. This is why currently more and more experts recommend it as a valuable therapeutic option for selected women who have undergone a careful risk-benefit analysis.
What does testosterone do in females?
Testosterone is often called the male sex hormone because it is an androgen (induces male-like characteristics), and it’s the predominant reproductive hormone in men.
Yet, some scientists suggest that testosterone can also be considered the predominant reproductive hormone in women, despite the fact that females have about 20 times lower levels than males.
The female body produces more testosterone than estrogens, such as estradiol, throughout its lifespan
Total testosterone levels in healthy adult women tend to revolve around 8-60 ng/dl, while estradiol levels are 5-40 ng/dl, depending on the phase of the menstrual cycle.
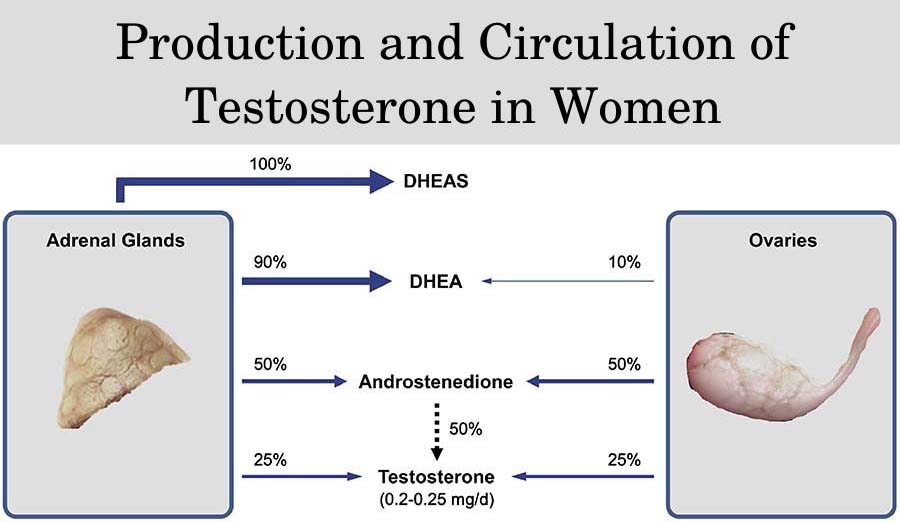
More specifically, women produce about 200 mcg to 300 mcg of testosterone per day on average. About a quarter of that amount is produced by the ovaries, while another quarter is produced by the adrenals.
The ovaries and the adrenals also produce other androgens, such as DHEA (dehydroepiandrosterone) and androstenedione. They get converted into testosterone by peripheral tissues, which contributes to the other 50% of T production.
However, it’s also important to note that the majority of that testosterone is bound to sex-hormone binding globulin (SHBG) and inactivated. Free T levels in women are within 0.06-1 ng/dl.
Testosterone has played a major role in women’s health since puberty when serum levels peak up to 75 ng/dl compared to prepubertal levels when they are under 20 ng/dl.
During puberty, T stimulates the development of sexual characteristics such as axillary and pubic hair growth. In adult women, testosterone plays a major role in regulating sexual desire, vaginal lubrication, mood, bone mineral density, and muscle development.
For example, clinical trials report that both estrogen and testosterone are required for maintaining bone mineral density and preventing osteoporosis in postmenopausal women.
Similar to men, low T in women can lead to problems with sexual desire, orgasms, bone health, cardiovascular health, mood, physical performance, etc.
Do women also have low T?
Women can have low testosterone, which is most commonly defined as total T levels under 8 ng/dl. However, this is not a widely accepted definition, and most experts disagree on the specific physiological ranges for T in women.
It is difficult to estimate the exact healthy range of T in women, considering that half of the hormone is produced peripherally from other androgens.
Therefore, there are still no diagnostic criteria for identifying low T in women. Testosterone levels are also not routinely checked in women, and the incidence of low T in females is currently unknown.
One of the most common causes of low T in women is surgical menopause, which occurs due to the surgical removal of the ovaries (ovariectomy). The procedure is performed as a life-saving intervention in women with certain cancers.
Due to the sudden decline in T levels, women undergoing surgical menopause often experience a lack of libido, hot flashes, night sweats, muscle weakness, and depression.
Other causes of low T in women include endocrine disorders (hypopituitarism, Cushing’s), long-term therapy with oral contraceptives, eating disorders (anorexia), and in HIV/AIDS.
T levels in women also naturally decline with age, especially during and after menopause, as the function of the ovaries shuts down.
The decrease in testosterone leads to symptoms such as:
- decreased sexual desire
- vaginal dryness and pain during intercourse
- unstable mood
- chronic fatigue
Low T can also increase the risk of serious complications in the long term, which have specific symptoms such as bone pain and a higher rate of fractures.
Should women take testosterone therapy?
Testosterone therapy is not officially approved for any indication in women. Nevertheless, TRT can be legally prescribed off-label if a medical doctor has decided that the benefits of the therapy will outweigh the potential risks.
One of the most common conditions treated with off-label TRT is hypoactive sexual desire disorder (HSDD).
Yet, it’s important to note that the condition is not related to testosterone levels, and it affects women regardless of whether they are pre- or postmenopausal. Moreover, TRT can help improve the symptoms of HSDD regardless of whether the treated women had normal or low serum testosterone.
More specifically, HSDD manifests with an absence of sexual fantasies or any desire for sexual activity
TRT can be used to improve libido in HSDD, but only for postmenopausal women. It may also help improve vaginal lubrication and sexual satisfaction.
Guidelines recommend against using TRT in premenopausal women due to a lack of research. Furthermore, TRT can suppress fertility in premenopausal women who are planning to have children in the future.
On the other hand, low-dose TRT appears to be well-tolerated in postmenopausal women as long as the dosages achieve serum levels within the physiological range.
The official recommendation by the International Society for the Study of Women’s Sexual Health is that TRT should be used in “postmenopausal women presenting with a decline in sexual interest with or without diminished arousal that causes sufficient personal or interpersonal concern (distress) that they seek treatment”.
More specifically, the latest guidelines recommend daily doses within the range of 150-300 mcg/day (micrograms per day).
What is the best form of testosterone for women?
According to the experts, the safety of such doses has been evaluated for up to 4 years, and there wasn’t any increase in serious adverse reactions such as cardiovascular events or cancer when compared to the general population.
Furthermore, the International Society for the Study of Women’s Sexual Health and the Endocrine Society both recommend that the most suitable forms of TRT for women are gels, creams, and patches.
They advise against the use of compounded testosterone, pellets, injections, and oral formulations of TRT due to the increased risk of side effects, rapid increase in serum testosterone, and difficulties in maintaining stable physiological T levels.
What happens when a woman starts taking testosterone?
The aim of TRT in women is to maintain serum testosterone levels within the upper physiological range and avoid achieving supraphysiological levels.
This is why medical specialists should monitor TRT in women closely and perform prophylactic examinations every 3-6 weeks.
Postmenopausal women taking TRT should expect improvements in libido, vaginal lubrication, and orgasms within 6 months of treatment.
After 6 months of therapy, the patients should be reevaluated, and they may continue taking TRT only if there are insignificant benefits.
What are the side effects of testosterone therapy for females?
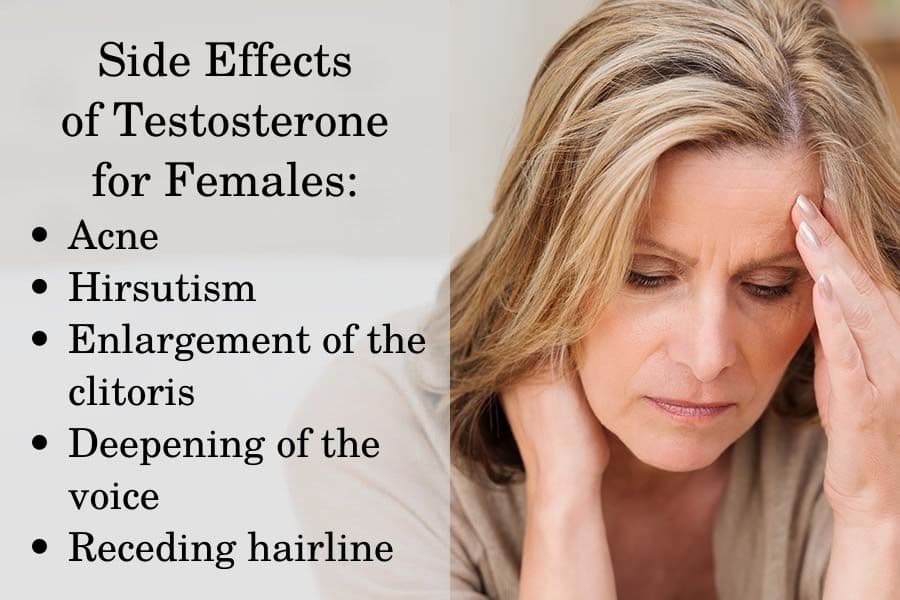
The side effects of TRT in women can be minimized by maintaining testosterone levels within the premenopausal range. However, when serum T levels exceed the normal references, it can lead to certain androgen-related adverse reactions.
The main side effects include acne, hirsutism (excessive body and facial hair growth), increased sweating and oily skin, enlargement of the clitoris, deepening of the voice, and androgenic alopecia (receding hairline).
Some of the side effects of testosterone, such as an enlarged clitoris, hair loss, hirsutism, and voice hoarseness, may persist in the long term, even after discontinuing the therapy.
Furthermore, trials have reported a reduction in the good cholesterol (HDL) along with a statistically significant increase in the bad cholesterol (LDL) with oral but not with transdermal testosterone preparations. Some forms of oral testosterone may also exert hepatotoxicity.
Transdermal testosterone appears to be the safest TRT option for women, as it rarely leads to supraphysiological serum T when dosed properly. This is why transdermal testosterone hasn’t been reported to cause any serious side effects. In fact, some studies on women who took testosterone gel reported no side effects at all.
One meta-analysis examined 7 trials with 3,035 participants who received transdermal testosterone 300 mcg or placebo and reported no risk of hair loss, clitoromegaly, deeper voice, or breast cancer. There was only a small increase in the risk of acne and body hair growth.
The researchers do not report an increased risk of mood swings during TRT. Furthermore, there appears to be a complex relationship between weight gain and testosterone therapy.
Physiological doses of testosterone in women do not appear to cause weight gain. Yet, higher body weight and weight management problems are common in women who have high testosterone levels due to diseases, such as polycystic ovary syndrome.
However, weight gain may be a causative factor rather than a result of the increase in serum T in such conditions.
Can testosterone therapy be beneficial for women?
Studies report several potential benefits of testosterone therapy in postmenopausal women with HSDD, including improved sexual desire, frequency of satisfying sexual events, arousal, orgasm frequency, pleasure, responsiveness, and self-image while reducing sexual concerns and personal distress.
Furthermore, testosterone therapy can increase sex drive in other conditions such as menopause (incl. surgical menopause), hypopituitarism, anorexia, HIV/AIDS, etc. Studies also report an increase in bone mineral density, increased muscle mass, and improvements in mood in those patients.
However, it’s important to note that many of the patients who experienced these benefits had T levels within reference despite their condition.
Therefore, the latest evidence on the use of TRT in women suggests that treatment should be initiated based on symptoms and diagnosis (such as HSDD in menopausal women) rather than on serum T levels. Instead, serum testosterone can be used for monitoring during therapy and reducing the risk of side effects.
TRT may also provide benefits for the brain and the cardiovascular system in postmenopausal women, although the evidence is still scarce.
Studies suggest that having higher T levels in women is linked to better memory, while low T may increase the risk of dementia. Nevertheless, more research is needed to evaluate the effect of testosterone on cognition in older women.
Having low T in postmenopausal women is also associated with an increased risk of atherosclerosis. Therefore, TRT may have benefits for cardiovascular health in females similar to those observed in males who receive physiological doses of testosterone.
Get a free consultation with our medical expert for any questions about hormone replacement therapy